Worried About Your Testicles? Understanding Pain, Lumps, Swelling, and Vasectomy
Let's talk openly about something that causes a lot of men significant worry: testicular health. Whether you've noticed pain, found a lump, seen some swelling, are considering a vasectomy, or just feel that something isn't quite right down there, it's completely natural to feel anxious. It’s a very private area, and discussing concerns can feel embarrassing or difficult.
As a Consultant Urologist, helping men understand and manage testicular conditions is a core part of my work. I see individuals every week with similar concerns to yours. My aim with this page is to demystify things – to give you clear, reliable information about common testicular issues, explain how we investigate them, detail procedures like vasectomy, hydrocele repair, and cyst removal, and critically, help you understand when you absolutely need to seek medical advice. Knowledge is power, and understanding what might be going on is the first step towards getting the right care and easing your mind. Rest assured, many testicular conditions are benign (not cancer) and treatable, but prompt assessment is key, especially for certain symptoms. Your wellbeing and comfort are my priority, and I strive to create a supportive environment where you feel heard and respected, regardless of your background or identity.
First Things First: Understanding Your Testicular Anatomy & How They Got There
Before diving into problems, let's quickly cover the basics. Your testicles (or testes) are the two oval-shaped glands hanging in the scrotum. They have two main jobs: making sperm for fertility and producing testosterone, the main male hormone. They are delicate but have several structures around them for support and function.
The Key Players Down Below: A Closer Look
Understanding the basic components helps make sense of potential issues:
- The Testicles (Testes): These are the primary reproductive organs in men. They contain tightly coiled tubes called seminiferous tubules where sperm are produced (spermatogenesis). Between these tubules are Leydig cells, which produce testosterone under the influence of Luteinising Hormone (LH) from the pituitary gland. Healthy adult testes are typically firm but slightly yielding, smooth, and roughly 4-5cm long.
- The Epididymis: This is a C-shaped, tightly coiled tube attached to the back of each testicle. It acts like a finishing school and storage depot for sperm. Sperm produced in the testis travel into the epididymis where they mature over several weeks, gaining the ability to swim (motility). The epididymis can be felt as a soft, comma-shaped structure; it's a common site for cysts and inflammation (epididymitis).
- The Spermatic Cord: This is the 'lifeline' structure running from the abdomen down to each testicle. It contains:
- The Vas Deferens (or Ductus Deferens): A muscular tube that transports mature sperm from the epididymis up towards the urethra during ejaculation. This is the tube cut or blocked during a vasectomy.
- Blood Vessels: The testicular artery supplies oxygenated blood, while a network of veins (the pampiniform plexus) drains blood away. This plexus helps cool the blood before it reaches the testis, essential for optimal sperm production (testes need to be slightly cooler than core body temperature). Issues here can lead to varicoceles.
- Nerves and Lymphatics: Providing sensation and fluid drainage.
- The spermatic cord is what twists during testicular torsion.
- The Scrotum: The sac of skin and muscle (dartos muscle) that holds the testicles, epididymis, and lower spermatic cords. Its ability to contract (pulling testes closer to the body for warmth) and relax (letting them hang lower to cool) helps regulate testicular temperature. It has several layers derived from the abdominal wall layers during development.
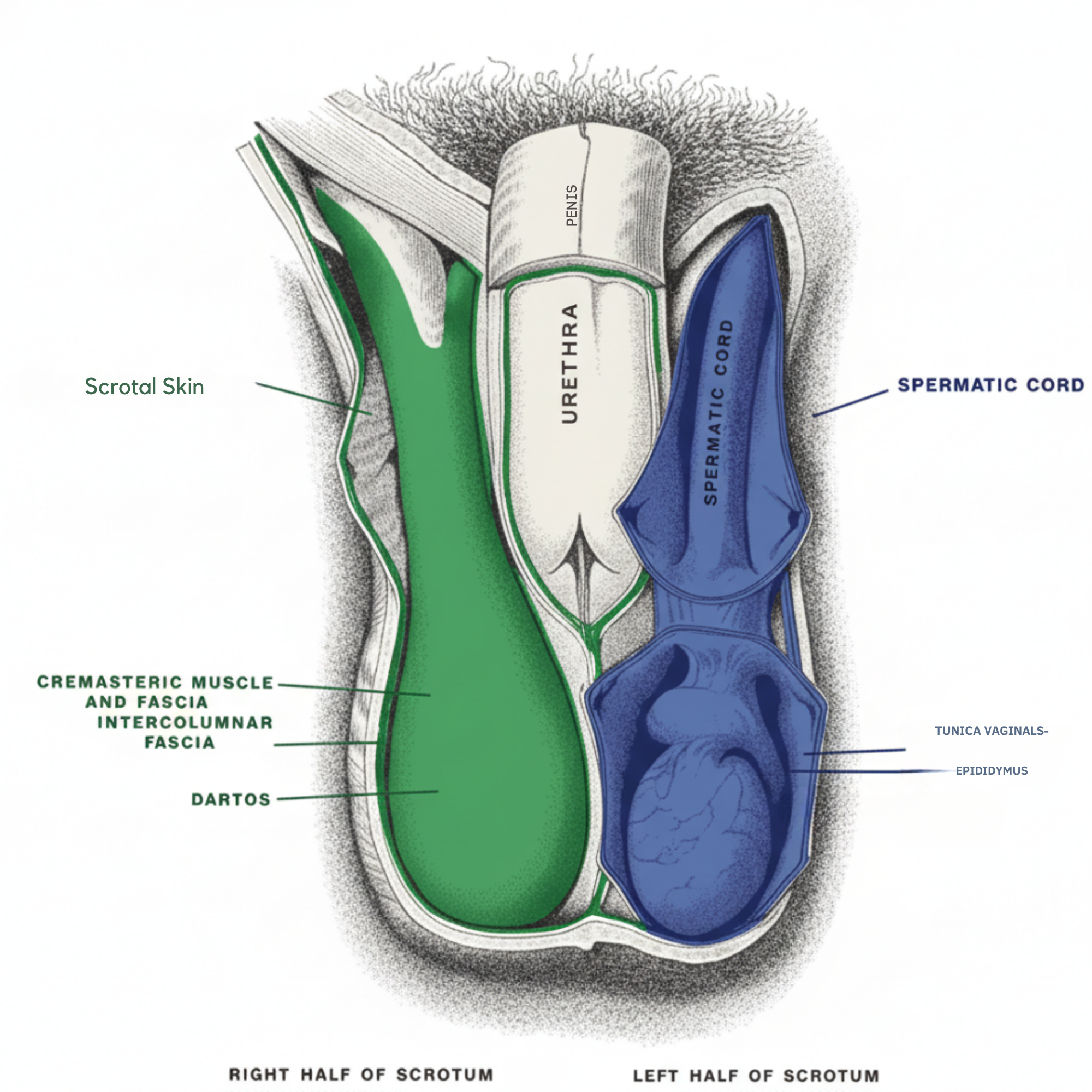
Simplified anatomical illustration of the male scrotal region
The Journey Downstairs: Testicular Development and Descent
Testicles don't start in the scrotum. In a developing male fetus, they form high up in the abdomen, near the kidneys. Guided by hormonal signals and anatomical structures, they gradually descend through the abdomen, pass through a passage in the groin called the inguinal canal, and (usually) reach their final destination in the scrotum by the time of birth or shortly after. This journey is crucial for normal function later in life.
What Are Undescended Testes?
Cryptorchidism is the medical term for when one or both testicles fail to complete their descent into the scrotum. It's one of the most common genital abnormalities in newborn boys, affecting around 3-4% of full-term infants and up to 30% of premature infants. In many cases, the testicle(s) will descend naturally within the first few months of life (usually by 6 months).
Why Does it Matter if a Testicle Doesn't Descend?
If a testicle remains outside the scrotum (e.g., in the groin or abdomen), it's exposed to a higher body temperature. This is significant because:
- Impaired Fertility: The higher temperature can damage the sperm-producing cells over time, potentially reducing fertility later in life, especially if both testes are affected or if treatment is delayed.
- Increased Risk of Testicular Cancer: Men born with undescended testes have a higher lifetime risk of developing testicular cancer in that testicle (even after surgical correction), although the overall risk is still low. Bringing the testicle down allows for easier self-examination and monitoring.
- Increased Risk of Torsion: An undescended testicle may be more prone to twisting (torsion).
- Associated Hernia: An inguinal hernia (a bulge in the groin) is often present alongside an undescended testicle.
How Are Undescended Testes Managed? (Orchidopexy)
If a testicle hasn't descended by around 6 months of age, surgical intervention, called orchidopexy (or orchiopexy), is usually recommended. Waiting much longer can increase the risk of fertility problems.
- Timing: The optimal timing for surgery is generally considered to be between 6 and 12 months of age.
- The Surgery (Orchidopexy): This is typically a day-case procedure performed under general anaesthesia.
- For Palpable Testes (felt in the groin): A small incision is usually made in the groin crease to find the testicle and spermatic cord. The cord is carefully freed up (mobilised) to gain enough length. A second small incision is made on the scrotum, creating a small pouch. The testicle is then gently brought down into the scrotal pouch and secured (fixed) in place with stitches. Any associated hernia is usually repaired at the same time.
- For Non-Palpable Testes (cannot be felt): A laparoscopy ('keyhole surgery') is often performed first. A small camera is inserted through the belly button to locate the testicle inside the abdomen. If a healthy testicle is found, it can often be brought down in one or two stages using laparoscopic techniques or a standard groin incision approach. If the testicle is absent or very poorly formed, it might be removed laparoscopically.
- Post-operative Care: Recovery is usually straightforward. Pain relief is provided, and activities are restricted for a short period. Follow-up checks ensure the testicle remains in place and heals well.
Key Takeaway: Early identification and surgical correction (orchidopexy) of undescended testes are crucial for maximising fertility potential and allowing for testicular self-examination. If you notice your son's scrotum seems empty on one or both sides, seek assessment from a paediatrician or urologist.
Feeling Pain Down There? Understanding Acute vs. Chronic Testicular Pain
Pain in the testicle or scrotum is a very common reason for men to seek medical help, and it can range from a dull ache to sudden, excruciating agony. The most critical thing is to know the difference between pain that needs immediate, emergency attention and pain that can be assessed more routinely.
Sudden, severe pain in one testicle is a potential urological emergency. Time is critical, and you must seek help immediately (attend A&E - Accident & Emergency).
What is Testicular Torsion?
Imagine the testicle is hanging by the spermatic cord, which contains its blood supply. Torsion occurs when the testicle twists around on this cord, cutting off the blood flow like kinking a hosepipe. Without blood, the testicular tissue rapidly starts to die (infarction).
Clinical Presentation (What it Feels/Looks Like):
- Sudden, severe pain in one testicle, often waking the patient from sleep.
- Pain may radiate to the lower abdomen or groin.
- Swelling and redness of the affected side of the scrotum.
- Nausea and vomiting are common due to the severity of the pain.
- The affected testicle may appear higher-riding than the other and may be lying horizontally ('bell clapper' deformity).
- Most common in adolescents and young adults but can occur at any age.
WARNING - TIME IS TESTICLE: If you suspect testicular torsion, do NOT 'wait and see'. Go immediately to your nearest A&E. There is roughly a 6-hour window from the onset of pain to surgically untwist the testicle (detorsion) with a high chance of saving it. Delays significantly increase the likelihood of irreversible damage requiring testicle removal (orchidectomy).
Emergency Surgical Exploration:
Diagnosis is often made clinically based on the story and examination, but sometimes an urgent Doppler ultrasound scan is performed in A&E if available quickly, to check blood flow. However, surgery should not be delayed if torsion is strongly suspected.
- The Operation: This is performed under general anaesthetic. An incision is made in the scrotum. The surgeon inspects the affected testicle. If torsion is confirmed, the testicle is untwisted (detorsion). If it appears viable (regains colour/bleeding), it is fixed (orchidopexy) with stitches to the inside of the scrotum to prevent it from twisting again. Crucially, the other (contralateral) testicle is also fixed during the same operation, as the anatomical variation allowing torsion often affects both sides. If the twisted testicle is clearly non-viable (dead), it will need to be removed (orchidectomy).
What is Epididymo-orchitis?
This refers to inflammation or infection of the epididymis (epididymitis) and/or the testicle itself (orchitis). It's a much more common cause of testicular pain than torsion.
Clinical Presentation (How it Differs from Torsion):
- Pain usually develops more gradually over hours or days, rather than minutes.
- Pain can range from mild to severe.
- Swelling and tenderness are often localised to the back of the testicle initially (epididymis) but can involve the whole structure.
- The scrotum may be red and warm.
- There might be associated symptoms like fever, urinary symptoms (burning, frequency), or discharge from the penis (especially in younger men, suggesting a sexually transmitted infection - STI).
Causes and Medical Management:
In younger, sexually active men (typically under 35), epididymo-orchitis is often caused by STIs like Chlamydia or Gonorrhoea. In older men, it's more commonly associated with urinary tract infections (UTIs) caused by bacteria spreading from the bladder or prostate.
Important Note: While less time-critical than torsion, suspected epididymo-orchitis still needs prompt medical assessment (GP or urgent care centre) to confirm the diagnosis, rule out torsion definitively (sometimes requiring ultrasound), and start appropriate treatment.
- Diagnosis: Based on history, examination, urine tests (to check for infection and culture bacteria), and sometimes STI screening (urethral swab or urine test). Ultrasound can help confirm inflammation and rule out torsion or abscess.
- Treatment: Primarily medical:
- Antibiotics: Chosen based on the likely causative organism (e.g., different antibiotics for suspected STI vs. UTI). A full course is essential.
- Pain Relief: Anti-inflammatory medications (like ibuprofen) and simple painkillers (paracetamol).
- Support: Scrotal support (e.g., supportive underwear) can help ease discomfort.
- Rest: Advisable during the acute phase.
- Most cases resolve well with antibiotics, but recovery can take several weeks. Complications like abscess formation or chronic pain are possible but less common.
Comparing Torsion and Epididymo-orchitis:
*Cremasteric reflex: Stroking the inner thigh causes the testicle on that side to lift – often lost in torsion. Examination finding for clinicians.
When the Ache Doesn't Go Away: Chronic Orchialgia
Chronic testicular pain, also known as orchialgia or chronic scrotal content pain, is defined as constant or intermittent testicular/scrotal pain lasting for three months or longer, significantly affecting the patient's quality of life.
Causes and Evaluation: Why Does it Happen?
Frustratingly, in many cases, a specific cause for chronic testicular pain cannot be identified (idiopathic orchialgia). However, potential contributing factors include:
- Post-infection changes: Lingering inflammation or nerve sensitivity after epididymo-orchitis.
- Post-surgical pain: Following vasectomy (Post-Vasectomy Pain Syndrome - PVPS), hernia repair, or other scrotal surgery.
- Nerve-related issues: Nerve entrapment or irritation in the groin or spermatic cord (e.g., genitofemoral nerve).
- Varicocele: Though less common, large varicoceles can sometimes cause a dull ache.
- Interstitial cystitis/Painful bladder syndrome: Pain can sometimes refer to the scrotum.
- Musculoskeletal causes: Pain referred from the back or hip.
- Psychological factors: Stress and anxiety can sometimes manifest as or exacerbate physical pain.
Evaluation is crucial to rule out any underlying treatable pathology. This involves:
- Detailed history of the pain (onset, character, triggers, relieving factors).
- Thorough physical examination, including scrotal contents, groin, and sometimes abdomen/back.
- Urine tests to exclude infection.
- Scrotal ultrasound to rule out structural abnormalities (cysts, tumours, varicoceles) and assess testicular tissue.
- Sometimes, further investigations like MRI or specialised nerve tests might be considered.
Management: A Challenging Condition
Treating chronic testicular pain can be challenging and often requires a multi-modal approach. Patience is key, as finding effective relief can take time.
- Conservative Measures: Supportive underwear, heat/cold packs, lifestyle adjustments (avoiding triggers).
- Medical Therapy:
- Painkillers: Simple analgesics (paracetamol) and anti-inflammatories (NSAIDs).
- Nerve Pain Medications: Drugs typically used for nerve pain, like amitriptyline, gabapentin, or pregabalin, may be helpful, started at low doses.
- Antibiotics: Sometimes a prolonged course is tried if post-infectious inflammation is suspected, though evidence is limited.
- Injections: Spermatic cord blocks (injecting local anaesthetic, sometimes with steroid, around the nerves in the cord) can provide temporary or sometimes longer-lasting relief and help diagnostically.
- Pelvic Floor Physiotherapy: Can be beneficial if muscular tension is contributing.
- Psychological Support/Pain Management Programmes: Addressing coping strategies, anxiety, and depression associated with chronic pain.
- Surgical Options (Considered Carefully):
- Microsurgical Denervation of the Spermatic Cord (MDSC): A specialised procedure to carefully divide the nerve fibres in the spermatic cord while preserving the blood supply and vas deferens. Reserved for severe, refractory pain where cord blocks provide temporary relief.
- Epididymectomy (Removal of Epididymis): Considered if pain seems clearly localised to the epididymis (e.g., chronic epididymitis, post-vasectomy pain).
- Orchidectomy (Testicle Removal): A last resort for debilitating pain unresponsive to all other measures, with no guarantee of complete pain relief as 'phantom' pain can persist. Requires extensive counselling.
- Varicocelectomy: If a varicocele is present and thought to be the source of the ache (discussed further on our Varicocele page).
Managing chronic testicular pain often involves working closely with a urologist specialising in male pain conditions and potentially a multidisciplinary pain team.
Found a Lump or Swelling? What Could it Be?
Discovering a lump, bump, or swelling in the scrotum is understandably alarming for most men, with the immediate fear often being cancer. While it's absolutely vital to get any new lump checked out promptly by a doctor, it's reassuring to know that the vast majority of scrotal lumps are benign (non-cancerous).
Regular self-examination is key to noticing changes early.
Know Your Nuts: A Simple Guide to Self-Exam
Checking your testicles regularly (ideally monthly) helps you become familiar with what's normal for you, making it easier to spot any changes early. The best time is often during or after a warm bath or shower when the scrotal skin is relaxed.
- Get Comfortable: Stand in front of a mirror if possible. Check for any visible swelling on the scrotal skin.
- Examine Each Testicle Separately: Use both hands. Place your index and middle fingers under the testicle and your thumbs on top.
- Roll Gently: Gently roll the testicle between your thumbs and fingers. Don't squeeze hard. Familiarise yourself with its size, shape, and consistency – it should feel smooth, oval-shaped, and fairly firm but not rock-hard. It's normal for one testicle to be slightly larger or hang lower than the other.
- Feel the Epididymis: At the back of the testicle, you should feel the soft, tube-like structure of the epididymis. It can feel a bit lumpy or tender normally – learn what feels normal for you here, as this is where harmless cysts often form.
- Check for Lumps or Changes: Feel for any hard lumps, smooth rounded bumps, or changes in the size, shape, or consistency of the testicle itself.
- Repeat on the Other Side.
What to look out for:
- A hard lump on the front or side of the testicle.
- Swelling or enlargement of one testicle.
- An increase in firmness.
- A feeling of heaviness in the scrotum.
- A dull ache in the lower abdomen, groin, or scrotum (though pain is less common with cancer lumps).
Found Something? Don't Panic, But Do Act: If you notice any lump, swelling, hardness, pain, or anything unusual during your self-exam, make an appointment to see your GP or a urologist promptly. Early detection is key for all conditions, especially testicular cancer.
These conditions are far more common than testicular cancer:
What is a Hydrocele?
A hydrocele is a collection of clear fluid in the sac (tunica vaginalis) that naturally surrounds the testicle, causing smooth, often painless scrotal swelling.
Causes and Presentation:
Often develops slowly without cause (idiopathic) in adults, but can follow inflammation or injury. In infants, often linked to a connection with the abdomen. The swelling is typically soft, non-tender, and light shines through it (transilluminates).
Management and Surgical Repair (Hydrocelectomy)
Small, asymptomatic hydroceles often don't need treatment. Surgery (hydrocelectomy) is effective for large, bothersome hydroceles.
Pre-operative Preparation:
- Consultation: Discussion of symptoms, confirmation of diagnosis (usually with ultrasound), explanation of the procedure, risks, benefits, and alternatives. Decision to proceed is made together.
- Anaesthetic Assessment: Review of medical history to ensure fitness for anaesthesia (usually general or spinal, sometimes local with sedation).
- Medications: You'll be advised about stopping blood-thinning medications (like aspirin, clopidogrel, warfarin, NOACs) for a specific period before surgery.
- Fasting: Instructions on when to stop eating and drinking before the operation will be given.
Intra-operative (During Surgery):
- Anaesthesia: Administered by the anaesthetist for comfort and stillness.
- Positioning: Lying on your back. The genital area is cleaned with antiseptic.
- Incision: A small incision (typically 3-5 cm) is made on the affected side of the scrotum, often within a natural skin crease.
- Dissection & Delivery: The surgeon carefully dissects through the scrotal layers to expose the swollen hydrocele sac containing the testicle. The testicle and sac are delivered out through the incision.
- Fluid Drainage & Sac Management: The sac is opened, and the straw-coloured hydrocele fluid is drained. The redundant sac lining (tunica vaginalis) is then managed to prevent fluid re-accumulating. Common techniques include:
- Excision: Trimming away the excess sac lining.
- Plication/Eversion (Lord's or Jaboulay's): Turning the sac inside-out and stitching it behind the testicle.
- Haemostasis: Careful control of any bleeding points is ensured.
- Drain (Optional): A small, soft drain tube may be placed temporarily to remove any residual fluid or blood, usually removed before discharge or shortly after.
- Closure: The testicle is returned to the scrotum. The scrotal layers and skin are closed meticulously with dissolvable stitches. A supportive dressing is applied.
Post-operative Recovery & Care:
- Immediate Recovery: Monitored in the recovery room as anaesthesia wears off. Pain relief is given.
- Discharge: Most patients go home the same day (day case) once comfortable, mobilising, and able to pass urine.
- Pain Management: Regular painkillers (paracetamol, ibuprofen if suitable) are usually sufficient. Stronger medication may be provided if needed initially.
- Swelling and Bruising: Expect significant scrotal swelling and bruising. This is normal and can take several weeks, sometimes 2-3 months, to fully resolve. The scrotum might initially look larger than before surgery!
- Scrotal Support: Wearing supportive underwear (e.g., snug briefs or an athletic support) continuously for the first 1-2 weeks is crucial to minimise swelling and discomfort.
- Ice Packs: Applying ice packs (wrapped in a thin towel) intermittently (e.g., 15-20 minutes every few hours) during the first 24-48 hours can help reduce swelling.
- Wound Care: Keep the incision clean and dry. Showering advice will be given (often okay after 48 hours, pat dry gently). Avoid bathing until advised. Dissolvable stitches disappear on their own.
- Activity: Rest for the first few days. Avoid strenuous activity, heavy lifting (>5kg), and vigorous exercise for at least 2-4 weeks, or as advised by your surgeon.
- Driving: Usually avoided for 1-2 weeks, until comfortable performing an emergency stop and no longer taking strong painkillers. Check with your insurance provider.
- Sexual Activity: Usually advised to wait 3-4 weeks, or until discomfort and swelling have significantly settled.
- Work: Return to work depends on the job type – typically 1-2 weeks for office jobs, 3-4 weeks or longer for manual labour.
- Follow-up: An appointment is usually scheduled a few weeks post-surgery to check healing and address any concerns.
- Potential Complications: While generally safe, risks include infection, bleeding (haematoma - collection of blood), recurrence of the hydrocele (uncommon with modern techniques), chronic pain, injury to testicular structures (rare), and anaesthetic risks. Seek medical advice if you experience increasing pain, fever, wound discharge, or rapidly expanding swelling.
What are Epididymal Cysts and Spermatoceles?
These are very common, benign (harmless) fluid-filled sacs within the epididymis (the tube behind the testicle), feeling like smooth, distinct lumps separate from the testicle. An epididymal cyst contains clear fluid, while a spermatocele contains cloudy fluid with sperm. They feel identical on examination.
Management: Usually Just Reassurance
Most require no treatment. They are harmless and don't affect fertility or become cancerous. Ultrasound confirms the diagnosis. Surgery (excision) is reserved only for rare cases where cysts are very large, persistently painful, or diagnosis is uncertain.
Why Surgery is Less Common:
Excision of epididymal cysts is performed less frequently than hydrocelectomy because the cysts are intrinsically harmless, and surgery carries a slightly higher risk profile due to the delicate nature of the epididymis. Potential risks include chronic pain, recurrence, infection, bleeding, and, importantly, potential damage or scarring to the epididymis which could theoretically affect sperm transport on that side (though often fertility is unaffected if the other side is normal).
Pre-operative Preparation:
- Similar to hydrocelectomy: Consultation including thorough discussion of risks/benefits, decision-making based on significant symptoms, anaesthetic assessment, medication adjustments, fasting. Consent emphasises the higher risk of chronic pain and potential fertility impact.
Intra-operative (During Surgery):
- Anaesthesia: Usually general or spinal anaesthesia.
- Incision & Exposure: A scrotal incision is made, and the testicle with the epididymis is delivered.
- Cyst Identification & Dissection: The cyst(s) on the epididymis are carefully identified. Using fine instruments (sometimes magnification loupes or microscope), the surgeon meticulously dissects the cyst away from the delicate epididymal tubules. The goal is to remove the cyst sac entirely while preserving the integrity of the epididymis. This can be challenging if the cyst wall is thin or adherent.
- Haemostasis & Closure: Bleeding points are controlled. The testicle is returned to the scrotum, and the layers are closed, typically with dissolvable stitches. A drain is less commonly used than for hydrocelectomy.
Post-operative Recovery & Care:
- Recovery is generally similar to hydrocelectomy regarding pain management, scrotal support, ice, wound care, and activity restrictions.
- Swelling and bruising are expected but may be less dramatic than after hydrocelectomy if the cyst was small.
- Emphasis on reporting any signs of infection or excessive swelling.
- Follow-up is arranged to check healing.
- Potential Complications: Risks include infection, bleeding/haematoma, recurrence (if the sac wasn't fully removed or new cysts form), chronic scrotal or epididymal pain (a recognised risk), damage to the epididymis affecting fertility, and anaesthetic risks.
Important Consideration: Due to the potential risks, particularly chronic pain, surgery for epididymal cysts is typically only recommended when the benefits of alleviating significant symptoms clearly outweigh these risks. Many men choose to live with asymptomatic cysts once reassured they are benign.
What is a Varicocele?
A varicocele is an enlargement of the veins draining the testicle, similar to varicose veins in the leg, usually occurring on the left side. They feel like a 'bag of worms' above the testicle.
Why Does it Matter?
Varicoceles are common (affecting ~15% of men). While many cause no issues, they can sometimes cause a dull ache or dragging sensation. Significantly, they are a known cause of male infertility in some individuals, likely by impairing testicular cooling and affecting sperm production and quality.
Management:
Treatment (surgical repair or radiological embolisation) is typically considered for bothersome symptoms (pain), testicular size difference in adolescents, or as part of managing male infertility when semen parameters are abnormal.
Want to know more? For a detailed explanation of varicocele diagnosis, grading, impact on fertility, and treatment options including microsurgical varicocelectomy, please visit our dedicated Varicocele Information Page.
What You Need to Know About Testicular Cancer
Testicular cancer is the most common cancer in young men, typically affecting those between the ages of 15 and 40, although it can occur at any age. The good news is that it's also one of the most curable forms of cancer, especially when detected early. Cure rates exceed 95% overall.
Risk Factors and Presentation:
Known risk factors include:
- Undescended testicle (cryptorchidism): Even if surgically corrected.
- Family history of testicular cancer.
- Previous testicular cancer in the other testicle.
- Certain genetic conditions (less common).
- Subfertility is also associated with a slightly increased risk.
The most common presentation is:
- A painless lump or swelling *within* the testicle itself.
- An increase in firmness or hardness of the testicle.
- A feeling of heaviness in the scrotum.
- Less commonly, dull ache, sharp pain, or symptoms from spread (metastasis) like back pain, cough, or swollen lymph nodes (rare at presentation).
Diagnosis and Why Ultrasound is Key:
If testicular cancer is suspected based on examination:
- Scrotal Ultrasound: This is the cornerstone investigation. It's highly accurate at distinguishing between lumps arising *within* the testicle (suspicious for cancer) and those outside it (like epididymal cysts or hydroceles, usually benign).
- Tumour Markers: Blood tests for specific proteins (Alpha-fetoprotein - AFP, human Chorionic Gonadotropin - hCG, Lactate Dehydrogenase - LDH) that can be elevated in certain types of testicular cancer. These help with diagnosis, staging, and monitoring treatment response.
- Staging Scans: If cancer is confirmed or highly suspected, CT scans of the chest, abdomen, and pelvis are usually performed to check if the cancer has spread (metastasised) to lymph nodes or other organs.
CRITICAL POINT: Biopsy through the scrotum is NOT done. If cancer is suspected, the standard procedure is removal of the entire testicle through the groin (inguinal orchidectomy) to prevent potential seeding of cancer cells into the scrotum.
Inguinal Orchidectomy: The Surgical Approach
If investigations strongly suggest testicular cancer, the primary treatment is surgical removal of the affected testicle and spermatic cord. This procedure is called a radical inguinal orchidectomy.
- Performed under general anaesthesia.
- An incision is made in the groin (like a hernia repair incision), *not* on the scrotum.
- The spermatic cord is identified and clamped high up near the internal inguinal ring to control blood vessels and prevent tumour cell spread.
- The testicle and entire spermatic cord are removed through the groin incision.
- The tissue is sent to pathology for detailed analysis to confirm the cancer type and extent.
- At the time of surgery, insertion of a testicular prosthesis (artificial testicle) can often be performed through the same incision if desired for cosmetic reasons (discussed beforehand).
Life After Orchidectomy and Further Treatment:
Removal of one testicle generally does not affect sexual function or fertility significantly, as the remaining testicle usually produces enough testosterone and sperm. However, fertility preservation (sperm banking) is strongly recommended *before* orchidectomy and any subsequent treatments (like chemotherapy or radiotherapy), especially as subfertility can pre-exist.
Following surgery and confirmation of the cancer type and stage (based on pathology and staging scans), further management is decided by a specialist multidisciplinary team (MDT) and may involve:
- Surveillance: For early-stage cancers, close monitoring with regular blood tests, scans, and check-ups may be all that's needed.
- Chemotherapy: Highly effective for testicular cancer that has spread or for certain types/stages to reduce the risk of recurrence.
- Radiotherapy: Sometimes used for a specific type called seminoma that has spread to nearby lymph nodes.
- Further Surgery: Rarely, removal of lymph nodes at the back of the abdomen (Retroperitoneal Lymph Node Dissection - RPLND) might be required.
With timely diagnosis and appropriate treatment tailored by experts, the outlook for testicular cancer is excellent.
Myth
Finding a scrotal lump automatically means it's cancer."
Fact
Absolutely not! While testicular cancer is the most serious cause, benign conditions like hydroceles, epididymal cysts, and varicoceles are far more common. However, only a medical evaluation (including examination and often an ultrasound) can determine the cause. Never ignore a new lump – get it checked promptly.
Myth
Testicular cancer is typical after 60 years of age
Fact
Definetly not! the typical age when most frequently testicular cancer is diagnosed is between 15 and 35 year of age. The good news is that it often is possible to cure it and an early diagnosi is the first step to it.
Considering Vasectomy? Permanent Contraception Explained
Vasectomy is a safe and highly effective method of permanent contraception for men who have completed their family or are certain they do not wish to father children in the future. It's a common procedure, but understanding exactly what it involves, its effectiveness, permanence, risks, and recovery is crucial before making this important decision.
The Basics of Vasectomy
Vasectomy works by blocking the tubes that carry sperm from the testicles to the penis. Remember the vas deferens we discussed in the anatomy section? That's the target. Sperm are still produced in the testicles after a vasectomy, but they can no longer travel through the vas deferens to mix with the seminal fluid during ejaculation.
Instead, the sperm are simply reabsorbed by the body, which is a natural and harmless process (similar to what happens with unused sperm normally). The procedure does not affect:
- Your testosterone levels (produced directly by the testicles into the bloodstream).
- Your sex drive (libido).
- Your ability to get an erection.
- The sensation of orgasm.
- The volume, colour, or appearance of your ejaculate fluid (semen) - sperm make up only a tiny fraction (about 2-5%) of the total volume. Most of the fluid comes from the seminal vesicles and prostate gland, which are unaffected.
Think of it like closing the gate (vas deferens) between the sperm factory (testicles) and the exit route, while everything else continues to function normally.
How is a Vasectomy Performed?
Vasectomy is typically a quick procedure (often 15-30 minutes) performed in an outpatient clinic or day surgery setting, usually under local anaesthesia, meaning you'll be awake but the area will be completely numb.
Anaesthesia:
- Local Anaesthetic: This is the most common method. A fine needle is used to inject anaesthetic solution into the skin of the scrotum and around each vas deferens. You might feel a brief sting, but the area quickly becomes numb. Some surgeons use 'no-needle' jet injectors for the initial skin numbing. Sedation is rarely required but can be discussed if you are particularly anxious.
Surgical Techniques:
There are two main approaches to accessing the vas deferens:
- Conventional Vasectomy: One or two small incisions (cuts) are made in the scrotum with a scalpel to reach each vas deferens.
- No-Scalpel Vasectomy (NSV): This technique is increasingly preferred by many surgeons due to potentially lower rates of bleeding and infection. Instead of cutting, the surgeon uses a special pointed instrument to make a tiny puncture hole in the scrotal skin. The vas deferens is gently stretched and brought out through this small opening. Often, both vasa can be accessed through a single central puncture.
Blocking the Vas Deferens:
Once accessed, each vas deferens is blocked. There are several methods surgeons use, often in combination:
- Division: The vas is cut.
- Ligation: The cut ends are tied with sutures or clipped with tiny metal clips.
- Excision: A small segment of the vas may be removed.
- Fascial Interposition: A layer of tissue sheath surrounding the vas is stitched over one or both cut ends to create a barrier between them, further reducing the chance of them rejoining (recanalisation).
- Cautery: Heat is used to seal the inside lining (mucosa) of the cut ends.
Your surgeon will discuss their preferred technique with you.
Closure:
- With the no-scalpel technique, the tiny puncture hole often seals itself and may not require stitches.
- With the conventional technique, the small incision(s) are usually closed with one or two dissolvable stitches.
- A dressing is applied, and supportive underwear is recommended immediately.
Confirming Success: Post-Vasectomy Semen Analysis (PVSA)
Vasectomy is highly effective (>99% successful at preventing pregnancy), but it is NOT effective immediately. Sperm can remain in the vas deferens 'downstream' from the blockage for several weeks or months after the procedure.
CRITICAL POINT: You MUST continue using other forms of contraception until you have provided semen samples for analysis and received confirmation from your doctor or clinic that the vasectomy has been successful (i.e., no sperm or only rare, non-motile sperm are seen).
The PVSA Process:
- You will be given instructions on when and how to produce semen samples after your vasectomy.
- Typically, the first sample is checked around 12 weeks after the procedure AND after you have had at least 20 ejaculations. This helps ensure the remaining sperm have been cleared out.
- The sample is examined under a microscope in a laboratory to look for the presence and motility (movement) of sperm.
- Clearance ('Special Clearance'): Is usually given when a sample shows azoospermia (no sperm at all) or only contains very small numbers of non-motile (dead) sperm, based on specific laboratory criteria and national guidelines (e.g., ASRM, EAU, FSRH guidelines in the UK often state <100,000 non-motile sperm/mL may be considered equivalent to azoospermia for clearance).
- Further Samples: If motile sperm are still present, or higher numbers of non-motile sperm, repeat samples will be required until clearance can be given.
- Persistent Motile Sperm: In a very small number of cases (early failure or recanalisation), motile sperm may persist, which might indicate the procedure needs repeating.
Following PVSA instructions carefully and achieving clearance is essential before relying on vasectomy for contraception.
Considering Permanence and Reversal
Vasectomy should always be considered a permanent form of contraception. While microsurgical vasectomy reversal (vasovasostomy or vasoepididymostomy) is possible, it is:
- Complex and Technically Demanding: Requires specialist microsurgical skills.
- Not Always Successful: Success rates (return of sperm to ejaculate and subsequent pregnancy) vary depending on factors like the time since vasectomy, the surgeon's experience, and whether epididymal blockage has occurred.
- Not Usually Available on the NHS: Reversal is typically self-funded privately and can be expensive.
Therefore, the decision to have a vasectomy should only be made if you are certain you do not want to father children in the future. Pre-vasectomy counselling should explore your circumstances, relationship status, and certainty about this decision.
Changing Circumstances? If your life situation changes significantly after vasectomy and you wish to explore fertility options, discuss this with a urologist specialising in male infertility and vasectomy reversal. Alternatives like sperm retrieval (from the testis/epididymis) combined with IVF/ICSI may also be an option, similar to managing obstructive azoospermia. For more on fertility challenges, see our Male Fertility Section or dedicated Infertility Hub Page.
Sperm banking *before* vasectomy is an option for men who want permanent contraception now but wish to keep open the possibility of fathering children later, although ongoing storage costs apply.
Understanding the Potential Downsides
While vasectomy is generally very safe, like any surgical procedure, it carries potential risks and complications, although serious ones are uncommon. These include:
- Short-Term (Usually within days/weeks):
- Bleeding/Haematoma: Collection of blood under the skin or around the testicle, causing significant swelling and bruising. Usually settles with rest, ice, support, but large haematomas might rarely require surgical drainage. Risk is low (<1%-5%), possibly lower with NSV.
- Infection: Infection of the skin wound or deeper structures (epididymitis/orchitis). Usually treated with antibiotics. Risk is low (around 1-2%).
- Mild Pain/Discomfort: Common in the first few days, managed with painkillers, ice, and support.
- Longer-Term (Potential):
- Sperm Granuloma: A small, sometimes tender lump caused by sperm leaking from the cut vas end. Usually harmless, may resolve spontaneously or require anti-inflammatories. Rarely needs excision if persistently painful.
- Congestion/Epididymitis: Some men experience temporary discomfort or inflammation in the epididymis due to sperm build-up shortly after the procedure; usually settles.
- Post-Vasectomy Pain Syndrome (PVPS): This is persistent or intermittent scrotal pain lasting for 3 months or more after vasectomy, significantly impacting quality of life. The cause is often unclear but may involve nerve irritation, chronic inflammation, or epididymal pressure. It affects a small percentage of men (estimates vary, perhaps 1-5% experience bothersome pain, severe debilitating pain is rarer). Management can be challenging and may involve medication, injections, or further surgery (like reversal or denervation) in refractory cases. Pre-vasectomy counselling should mention this possibility.
- Failure/Recanalisation: Very rarely, the cut ends of the vas deferens can spontaneously rejoin (early or late recanalisation), leading to vasectomy failure and the return of sperm to the ejaculate. This is why PVSA clearance is vital. The risk of failure after confirmed clearance is extremely low (estimated around 1 in 2000 or less).
Myth-Buster: "Vasectomy increases the risk of prostate cancer or heart disease."
Truth: Extensive research over many years has shown no credible link between vasectomy and an increased risk of prostate cancer, testicular cancer, cardiovascular disease, or other long-term health problems. Major medical organisations worldwide confirm vasectomy is a safe procedure in this regard.
Your surgeon will discuss these risks with you in detail during the consultation process.
Getting Ready: Key Considerations
Preparation involves both mental and practical steps:
- Consultation & Counselling: This is essential. You should have a clear discussion with the surgeon or counsellor covering:
- Confirmation that vasectomy is the right choice for you.
- Understanding that it is permanent contraception.
- Discussion of alternative methods (e.g., female sterilisation, long-acting reversible contraception like coils or implants).
- Explanation of the procedure technique, risks, benefits, failure rates, and the PVSA process.
- Assessment of your medical fitness.
- Opportunity to ask any questions.
- Written consent is required. You should feel entirely comfortable and informed before proceeding.
- Certainty: You must be sure about your decision. If you have any doubts, it's better to postpone and reconsider.
- Medications: Inform the surgeon about all medications you take, especially blood thinners. Adjustments may be needed.
- Scrotal Shaving: You will likely be asked to shave the scrotal area beforehand (or it may be done at the clinic) to allow for cleaning and clear access. Follow the specific instructions given.
- Arrange Transport: You should not drive yourself home immediately after the procedure, especially if you had any sedation or are feeling uncomfortable. Arrange for someone to collect you.
- Bring Supportive Underwear: Have snug-fitting briefs or an athletic support ready to wear immediately after the procedure.
Post-Vasectomy Care: Taking it Easy
Following the post-operative instructions carefully helps ensure a smooth recovery and minimises complications.
- Immediate Care: Rest quietly for the remainder of the day. Apply ice packs (wrapped) intermittently to the scrotum for 15-20 minutes at a time for the first 24-48 hours to reduce swelling and bruising.
- Pain Relief: Take regular simple painkillers like paracetamol. Ibuprofen or similar anti-inflammatories can also help with swelling, if suitable for you.
- Scrotal Support: Wear supportive underwear continuously (day and night initially) for the first few days, and then during the day for at least a week, or longer if comfortable.
- Rest & Activity: Take it easy for the first 2-3 days. Avoid heavy lifting, straining, strenuous exercise, sports, and cycling for at least 1-2 weeks, or as advised by your surgeon. Gradual return to normal activity.
- Wound Care: Keep the dressing clean and dry for the first 24-48 hours (follow specific instructions). Showering is usually okay after this, gently pat the area dry. Avoid soaking in a bath for about a week. Small wounds often need no further dressing; dissolvable stitches will disappear.
- Work: Most men return to office-based work after 2-3 days. Manual labourers may need a week or more off.
- Sexual Activity: Usually okay to resume after about a week, once discomfort has settled. Remember to use other contraception!
- PVSA Schedule: Crucially, follow the instructions precisely regarding when and how to provide your post-vasectomy semen samples for analysis (usually starting around 12 weeks post-op and after 20+ ejaculations). Continue other contraception until clearance is confirmed.
- Follow-up: Often not routine unless PVSA results are abnormal or you experience problems. Contact the clinic if you have concerns like increasing pain, fever, significant swelling, or wound discharge.
Most men experience only mild discomfort and recover quickly, but listening to your body and avoiding over-exertion initially is important.
Noticing Changes in Testicle Size or Feel?
Apart from distinct lumps or swelling, you might notice other changes in your testicles, like one seeming smaller than it used to, or a change in how firm it feels. While some size difference is normal, significant changes warrant investigation.
What Causes Testicles to Shrink?
Testicular atrophy refers to the shrinkage of a testicle. It implies damage to the sperm-producing tubules or the testosterone-producing Leydig cells, leading to a reduction in size and often firmness.
Potential causes include:
- Varicocele: A large varicocele can sometimes lead to ipsilateral (same side) testicular atrophy over time, particularly if it develops during adolescence.
- Aging: Testicular size and testosterone production can naturally decline slightly with age, though significant atrophy is not typical.
- Hormonal Imbalances: Low levels of pituitary hormones (FSH/LH) can lead to testicular shrinkage (secondary hypogonadism). Conversely, taking external testosterone or anabolic steroids shuts down the pituitary signals, causing the testes to shrink.
- Previous Torsion: Even if a testicle was saved after torsion, some degree of atrophy can occur later due to temporary oxygen deprivation.
- Previous Infection: Severe epididymo-orchitis, particularly mumps orchitis occurring after puberty, can damage testicular tissue.
- Undescended Testicle History: A previously undescended testicle may remain smaller than the normally descended one.
- Trauma: Significant injury can lead to atrophy.
Evaluation and Management:
If you notice significant testicular shrinkage, assessment is important to identify the underlying cause and check hormonal function. This usually involves:
- Clinical examination to assess size, consistency, and check for varicoceles.
- Scrotal ultrasound to measure volume accurately and assess tissue appearance.
- Hormonal blood tests (FSH, LH, Testosterone) to evaluate the pituitary-testicular axis.
- Semen analysis if fertility is a concern.
Management depends on the cause. For example, repairing a varicocele associated with atrophy in an adolescent might allow for some 'catch-up' growth. Treating underlying hormonal issues or stopping offending medications (like anabolic steroids) can sometimes allow recovery. If atrophy is associated with low testosterone causing symptoms (hypogonadism), testosterone replacement therapy might be considered (after addressing fertility, as TRT suppresses sperm production).
Restoring Appearance and Confidence: Artificial Testicles
For men who have lost a testicle (due to cancer, torsion, trauma, infection, or severe atrophy) or were born without one, the absence can sometimes cause psychological distress or issues with body image. A testicular prosthesis is a synthetic implant designed to mimic the look and feel of a natural testicle, restoring scrotal symmetry and fullness.
Indications and Considerations:
The main reason for prosthesis implantation is cosmetic and psychological benefit. The decision is entirely personal. Prostheses are available in various sizes to match the remaining testicle (if present).
Factors to discuss include:
- Timing (can often be done during the orchidectomy operation, or later as a separate procedure).
- Material (usually saline-filled silicone).
- Realistic expectations (it's for appearance/feel, it has no biological function).
- Risks (like infection, bleeding, pain, implant extrusion, scarring, dissatisfaction with position/feel, need for revision surgery – though complication rates are generally low).
Surgical Technique:
Implantation is typically a short procedure performed under general or local anaesthesia with sedation.
- If done during orchidectomy, it's placed through the same groin incision.
- If done later, a small incision is made either in the groin or upper scrotum.
- A pouch is created within the empty side of the scrotum.
- The prosthesis is inserted into the pouch and often secured with a stitch to the bottom of the scrotum to prevent it rotating or riding too high.
- The incision is closed in layers.
Outcomes:
Patient satisfaction rates are generally high, helping to restore confidence and body image. Recovery is usually quick, with scrotal support recommended for a few weeks.
Dealing with Testicular Trauma: Knocks, Blows, and Injuries
The testicles are sensitive, and injuries from sports, kicks, falls, or accidents can cause significant pain and swelling. Most minor bumps result in bruising that settles on its own, but more severe trauma needs urgent medical evaluation to rule out serious damage.
Assessment is Key After Injury
If you sustain a significant blow to the scrotum resulting in immediate, severe pain, significant swelling, bruising, nausea, or difficulty walking, you should seek urgent medical attention (A&E or urgent care).
Evaluation will involve:
- History: Understanding the mechanism and force of the injury.
- Examination: Assessing the degree of swelling, bruising (haematoma), tenderness, and crucially, whether the testicle itself feels intact.
- Scrotal Ultrasound: This is essential in significant trauma. It can:
- Visualise the testicle to check for rupture (fracture) of the tough outer capsule (tunica albuginea).
- Assess blood flow to rule out traumatic torsion or vascular injury.
- Estimate the size of any blood collection (haematocele) around the testicle.
- Check for injury to the epididymis.
Indications for Surgical Exploration:
While many cases of blunt trauma with an intact testicle on ultrasound can be managed conservatively (rest, ice, scrotal support, pain relief), surgery is indicated in certain situations:
- Testicular Rupture: If the ultrasound clearly shows a break in the tunica albuginea with extrusion of testicular contents. Prompt surgical repair offers the best chance of salvaging the testicle.
- Large or Expanding Haematocele: A large collection of blood around the testicle may require drainage to reduce pressure and pain, and allow inspection of the testis.
- Uncertain Ultrasound Findings / Persistent Suspicion: If the ultrasound is unclear but clinical suspicion of rupture remains high.
- Penetrating Trauma: Any injury that breaches the scrotal skin requires exploration.
Surgical Repair Techniques and Decision-Making:
Surgery is performed under general anaesthesia via a scrotal incision.
- The scrotum is opened, and any blood clot (haematocele) is evacuated.
- The testicle is carefully inspected.
- If a rupture (fracture) is found, any dead or extruded testicular tissue is gently removed (debrided).
- The tear in the tunica albuginea is repaired meticulously with absorbable stitches.
- The aim is to preserve as much viable testicular tissue as possible.
- A drain may be placed, and the scrotum is closed.
Salvage vs. Orchidectomy Decision:
The goal is always testicular salvage. However, in cases of severe trauma where the testicle is shattered beyond repair or its blood supply is irreversibly damaged, removal (orchidectomy) may unfortunately be necessary. This decision is made intra-operatively based on the extent of the damage.
Prompt evaluation and surgical intervention when indicated significantly improve the chances of saving an injured testicle and preserving its function.
How Can Testicular Conditions Affect Fertility?
Given that the primary function of the testicles is to produce sperm, it's logical that many of the conditions we've discussed can potentially impact male fertility. Understanding this link is important, especially for individuals planning a family or considering procedures like vasectomy.
The Testicle's Vital Role in Making Sperm
Optimal sperm production (spermatogenesis) requires healthy testicular tissue, the right hormonal signals (FSH, LH, Testosterone), and a slightly cooler temperature than the rest of the body. Various testicular conditions can disrupt this delicate process:
- Varicocele: As previously discussed, impaired cooling can impact sperm parameters. Significant varicoceles are a treatable cause of infertility in some men.
- Undescended Testicles (Cryptorchidism): Exposure to higher body temperatures damages sperm-producing cells, often leading to reduced fertility potential.
- Infection (Epididymo-orchitis): Inflammation can temporarily impair sperm production. Severe infections can cause scarring leading to blockage (obstructive azoospermia) or permanent testicular damage.
- Vasectomy: Intentionally causes obstructive azoospermia by blocking the vas deferens. Reversal is possible but complex and not always successful (see Male Infertility Hub).
- Testicular Torsion: Loss or damage to a testicle reduces sperm production capacity.
- Testicular Cancer & Treatment: The cancer itself and necessary treatments (surgery, chemotherapy, radiotherapy) can severely impact fertility. Sperm banking *before* treatment is crucial.
- Testicular Trauma: Significant injury can directly damage sperm-producing tissue.
- Hormonal Issues & Genetic Conditions: Directly disrupt sperm production signals or capability.
When Sperm Can't Get Out or Production is Severely Low: Surgical Sperm Retrieval (SSR)
For men facing infertility due to irreversible blockage (obstructive azoospermia - including post-vasectomy if reversal is not desired/possible) or severely impaired production (non-obstructive azoospermia), surgical sperm retrieval combined with IVF/ICSI offers a path to biological fatherhood.
Techniques aim to extract sperm directly from the epididymis or testis:
- PESA (Percutaneous Epididymal Sperm Aspiration): Needle aspiration from epididymis (mainly OA).
- MESA (Microsurgical Epididymal Sperm Aspiration): Microsurgical fluid collection from epididymal tubules (mainly OA).
- TESA (Testicular Sperm Aspiration): Needle aspiration from testis (OA or NOA).
- TESE (Testicular Sperm Extraction): Small open biopsy of testicular tissue (OA or NOA).
- Micro-TESE (Microsurgical Testicular Sperm Extraction): Gold standard for NOA, using a microscope to find pockets of sperm production.
Connection to Fertility Services: Successful SSR requires close collaboration between the urologist/andrologist and the IVF laboratory team for ICSI (Intracytoplasmic Sperm Injection). Retrieved sperm are often frozen (cryopreserved).
For a much more detailed discussion of male infertility investigation and treatment, including options after vasectomy, please see our dedicated Male Infertility Hub page.
Taking Charge of Your Testicular Health: When to Seek Help & What to Expect
Understanding the potential issues is the first step. Knowing when and how to act is the next. Don't hesitate to seek medical advice if you have concerns – your health is paramount.
Your Action Plan for Testicular Concerns:
- IMMEDIATE EMERGENCY (Go to A&E):
- Sudden, severe testicular pain.
- Significant testicular swelling occurring rapidly after trauma.
- Reason: Primarily to rule out testicular torsion where time is critical.
- URGENT APPOINTMENT (See GP or Urologist within days):
- Discovery of any new lump *within* the testicle itself (painless or painful).
- Significant, unexplained swelling or enlargement of a testicle.
- Noticeable increase in firmness or hardness of a testicle.
- Reason: To allow prompt investigation, particularly to rule out testicular cancer.
- ROUTINE APPOINTMENT (Book to see GP or Urologist):
- Gradual onset testicular pain or ache (after ruling out torsion).
- Lumps clearly separate from the testicle (e.g., suspected epididymal cyst).
- Large or bothersome hydrocele.
- Symptoms suggestive of a varicocele (dull ache, 'bag of worms' feel).
- Considering vasectomy or discussing vasectomy follow-up/concerns (e.g., PVPS).
- Concerns about testicle size or consistency (atrophy).
- General concerns about fertility related to testicular health.
- Discussion about previous conditions (e.g., undescended testis follow-up).
- Reason: To discuss concerns, get a diagnosis, plan appropriate management or reassurance, or discuss procedures like vasectomy.
Myth-Buster: "It's probably nothing, I don't want to bother the doctor or feel embarrassed."
Truth: Your health is never a bother. Doctors, especially urologists, deal with these concerns daily. Embarrassment is understandable, but delaying assessment for serious conditions like torsion or cancer can have life-altering consequences. Benign conditions can also cause worry, and getting a diagnosis provides peace of mind. Please, always get checked if you're concerned.
What to Expect After Common Procedures:
Recovery varies, follow your surgeon's specific advice. General guidelines:
Vasectomy:
- Anaesthesia: Local usually.
- Recovery: Minimal downtime. Rest 1-2 days. Ice packs, scrotal support, simple painkillers. Avoid heavy lifting/sports 1-2 weeks. Resume sex when comfortable (usually ~1 week). Use other contraception until PVSA clearance (typically 12+ weeks & 20+ ejaculations).
- More Detail: See the dedicated Vasectomy Recovery Section above.
Hydrocelectomy / Epididymal Cyst Excision:
- Anaesthesia: General/Spinal/Local+Sedation.
- Recovery: Day case usually. Significant swelling/bruising expected (weeks/months to settle). Scrotal support vital (1-2+ weeks). Ice initially. Regular painkillers. Avoid heavy lifting/straining 2-4 weeks. Driving/sex often 2-4 weeks+.
- More Detail: See expanded post-op sections under Hydrocele and Epididymal Cyst descriptions above.
Orchidopexy (Undescended Testis Repair):
- Anaesthesia: General (usually in childhood).
- Recovery: Day case usually. Mild discomfort. Small incisions. Limit rough activity few weeks.
Inguinal Orchidectomy (for Cancer):
- Anaesthesia: General.
- Recovery: Overnight stay typical. Groin incision pain. Avoid heavy lifting 4-6 weeks. Requires specialist follow-up/further treatment planning. Sperm banking essential beforehand.
Surgical Sperm Retrieval (TESE/Micro-TESE):
- Anaesthesia: General/Regional/Local+Sedation.
- Recovery: Day case. Scrotal discomfort/swelling/bruising. Painkillers, support. Avoid strenuous activity 1-2 weeks. Requires coordination with IVF unit.
Common Post-Op Advice Includes:
- Keep wounds clean and dry. Follow showering/bathing advice.
- Wear supportive underwear.
- Use ice packs (wrapped) as needed initially.
- Take pain relief regularly.
- Avoid constipation.
- Watch for signs of infection (increasing pain, redness, discharge, fever).
- Attend follow-up appointments.
You Are Not Alone: Finding Support
Dealing with testicular conditions, particularly cancer, chronic pain, infertility, or making decisions about procedures like vasectomy, can be emotionally challenging. Connecting with others and finding reliable information is key.
Consider exploring resources from reputable organisations (examples relevant to the UK):
- Orchid Cancer Appeal: Focuses on male cancers (testicular, penile, prostate). Offers information, support services, and raises awareness. [Placeholder: Link to Orchid website]
- Macmillan Cancer Support: Wide-ranging support for people affected by all cancers. [Placeholder: Link to Macmillan website]
- Cancer Research UK (CRUK): Reliable information about testicular cancer. [Placeholder: Link to CRUK website]
- Fertility Network UK: Support and information for fertility problems, including male factor infertility and post-vasectomy options. [Placeholder: Link to Fertility Network UK website]
- British Association of Urological Surgeons (BAUS): Patient information leaflets on urological conditions/procedures. [Placeholder: Link to BAUS Patient Information]
- Faculty of Sexual & Reproductive Healthcare (FSRH): Guidelines and patient information on contraception, including vasectomy. [Placeholder: Link to FSRH website]
Your GP or urology team may also be able to signpost you to local support services or specific counselling if needed (e.g., pre-vasectomy counselling, support for PVPS).
Remember: Seeking information from reliable sources and connecting with support networks can significantly help you navigate your health journey.
Experiencing Testicular pain during or after physical exercise?
Recently I operated a Personal Trainer that was suffering with a varicocele and he explained me how uncommon is the recognition of the problem in the sport communities. On reflection, it made perfectly sense and I decided to create a dedicated page to increase awareness and support who struggles right now.
Worried About Your Testicular Health or Considering Vasectomy? Let's Talk.
Understanding your body is the first step to taking control of your health. If you have concerns about testicular pain, lumps, swelling, size, fertility, or are considering vasectomy, please don't hesitate to seek expert advice. As a specialist in andrology and men's urological health, I'm here to provide discreet, comprehensive assessment and personalised care in London and Milton Keynes. Let's address your concerns together and find the right path forward for you.
The information presented on this page reflects current understanding and clinical guidelines in urology and andrology. For those seeking more detailed medical literature, key areas of research and guidelines include:
Core Guidelines
- European Association of Urology (EAU). Sexual and Reproductive Health (incl. Male Infertility). Arnhem: EAU Guidelines Office; 2024–2025 updates available online. uroweb.org
- European Association of Urology (EAU). Testicular Cancer. Arnhem: EAU Guidelines Office; 2024 update. uroweb.org
- European Association of Urology (EAU). Chronic Pelvic Pain (Pocket Guideline). Arnhem: EAU Guidelines Office; 2024. d56bochluxqnz.cloudfront.net
- American Urological Association (AUA), American Society for Reproductive Medicine (ASRM). Male Infertility: Guideline (latest amendment 2024). Linthicum, MD: AUA; 2024. healthbook.org
- American Urological Association (AUA). Diagnosis and Treatment of Early-Stage Testicular Cancer (2019; amended 2023; J Urol 2024 print). Linthicum, MD: AUA; 2023–2024. AUA
- American Urological Association (AUA). Vasectomy Guideline (2012; amended 2015). Linthicum, MD: AUA; 2015. AUA
- Faculty of Sexual & Reproductive Healthcare (FSRH). Male and Female Sterilisation. London: FSRH; Sept 2014 (current). CoSRH
- World Health Organization (WHO). Laboratory manual for the examination and processing of human semen. 6th ed. Geneva: WHO; 2021. World Health Organization
UK resources used in practice (where applicable)
- National Institute for Health and Care Excellence (NICE). Suspected cancer: recognition and referral (NG12). London: NICE; last updated 1 May 2025. NICE
- National Institute for Health and Care Excellence (NICE). Chronic pain in over 16s: assessment of all chronic pain and management of chronic primary pain (NG193). London: NICE; 2021. NICE
- British Association of Urological Surgeons (BAUS). Patient Information Leaflets (urology procedures). London: BAUS; current web collection (ongoing updates). BAUS
Textbook
- Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, Wein AJ, eds. Campbell-Walsh-Wein Urology. 12th ed. Amsterdam: Elsevier; 2020–2021. Elsevier Health
Journals routinely referenced on the page
- European Urology (Elsevier). European Urology
- The Journal of Urology (AUA/Wolters Kluwer). (See AUA testicular cancer guideline article above.) PubMed
- BJU International (BJUI) (Wiley). BJUI
- Fertility and Sterility (ASRM/Elsevier). (Examples include vasectomy and semen analysis methodology updates.) Fertstert
- Human Reproduction Update / Andrology / Journal of Sexual Medicine as topic-specific sources when indicated.
Dealing with testicular conditions, particularly cancer, chronic pain, infertility, or making decisions about procedures like vasectomy, can be emotionally challenging. Connecting with others and finding reliable information is key.
Consider exploring resources from reputable organisations (examples relevant to the UK):
Here is the updated list in English with the verified direct links for your website:
- Orchid Cancer Appeal: Focuses on male cancers (testicular, penile, prostate). Offers information, support services, and raises awareness. Orchid Official Website
- Macmillan Cancer Support: Wide-ranging support for people affected by all cancers, providing practical, medical, and financial support. Macmillan Official Website
- Cancer Research UK (CRUK): Reliable information and the latest research regarding testicular cancer and other urological malignancies. CRUK Testicular Cancer Section
- Fertility Network UK: Support and information for fertility problems, including male factor infertility and post-vasectomy options. Fertility Network UK Website
- British Association of Urological Surgeons (BAUS): Comprehensive patient information leaflets on a wide range of urological conditions and surgical procedures. BAUS Patient Information
- Faculty of Sexual & Reproductive Healthcare (FSRH): Clinical guidelines and patient information on contraception, including vasectomy and reproductive health. FSRH Official Website
Please note: This content is for educational purposes only and does not substitute for professional medical advice. Always consult with a qualified healthcare provider for diagnosis and treatment of medical conditions.
